Lipoproteins Can be Subdivided into Several Subcategories
In the continual search for better measures of cardiac risk, researchers in the 1980s decided to break down lipoprotein particles into sub-categories. One of these researchers is Dr. Ronald M. Krauss. Krauss published extensively on the association between lipoprotein size and cardiac risk, eventually concluding (source):
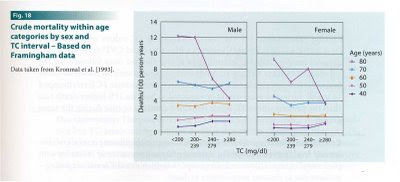
The plasma lipoprotein profile accompanying a preponderance of small, dense LDL particles (specifically LDL-III) is associated with up to a threefold increase in the susceptibility of developing [coronary artery disease]. This has been demonstrated in case-control studies of myocardial infarction and angiographically documented coronary disease.Krauss found that small, dense LDL (sdLDL) doesn't travel alone: it typically comes along with low HDL and high triglycerides*. He called this combination of factors "lipoprotein pattern B"; its opposite is "lipoprotein pattern A": large, buoyant LDL, high HDL and low triglycerides. Incidentally, low HDL and high triglycerides are hallmarks of the metabolic syndrome, the quintessential modern metabolic disorder.
Krauss and his colleagues went on to hypothesize that sdLDL promotes atherosclerosis because of its ability to penetrate the artery wall more easily than large LDL. He and others subsequently showed that sdLDL are also more prone to oxidation than large LDL (1, 2).
Diet Affects LDL Subcategories
The next step in Krauss's research was to see how diet affects lipoprotein patterns. In 1994, he published a study comparing the effects of a low-fat (24%), high-carbohydrate (56%) diet to a "high-fat" (46%), "low-carbohydrate" (34%) diet on lipoprotein patterns. The high-fat diet also happened to be high in saturated fat-- 18% of calories. He found that (quote source):
Out of the 87 men with pattern A on the high-fat diet, 36 converted to pattern B on the low-fat diet... Taken together, these results indicate that in the majority of men, the reduction in LDL cholesterol seen on a low-fat, high-carbohydrate diet is mainly because of a shift from larger, more cholesterol-enriched LDL to smaller, cholesterol-depleted LDL [sdLDL].In other words, in the majority of people, high-carbohydrate diets lower LDL cholesterol not by decreasing LDL particle count (which might be good), but by decreasing LDL size and increasing sdLDL (probably not good). This has been shown repeatedly, including with a 10% fat diet and in children. However, in people who already exhibit pattern B, reducing fat does reduce LDL particle number. Keep in mind that the majority of carbohydrate in modern America comes from wheat and sugar.
Krauss then specifically explored the effect of saturated fat on LDL size (free full text). He re-analyzed the data from the study above, and found that:
In summary, the present study showed that changes in dietary saturated fat are associated with changes in LDL subclasses in healthy men. An increase in saturated fat, and in particular, myristic acid [as well as palmitic acid], was associated with increases in larger LDL particles (and decreases in smaller LDL particles). LDL particle diameter and peak flotation rate [density] were also positively associated with saturated fat, indicating shifts in LDL-particle distribution toward larger, cholesterol-enriched LDL.Participants who ate the most saturated fat had the largest LDL, and vice versa. Kudos to Dr. Krauss for publishing these provocative data. It's not an isolated finding. He noted in 1994 that:
Cross-sectional population analyses have suggested an association between reduced LDL particle size and relatively reduced dietary animal-fat intake, and increased consumption of carbohydrates.Diet Affects HDL Subcategories
Krauss also tested the effect of his dietary intervention on HDL. Several studies have found that the largest HDL particles, HDL2b, associate most strongly with HDL's protective effects (more HDL2b = fewer heart attacks). Compared to the diet high in total fat and saturated fat, the low-fat diet decreased HDL2b significantly. A separate study found that the effect persists at one year. Berglund et al. independently confirmed the finding using the low-fat American Heart Association diet in men and women of diverse racial backgrounds. Here's what they had to say about it:
The results indicate that dietary changes suggested to be prudent for a large segment of the population will primarily affect [i.e., reduce] the concentrations of the most prominent antiatherogenic [anti-heart attack] HDL subpopulation.Saturated and omega-3 fats selectively increase large HDL. Dr. B. G. of Animal Pharm has written about this a number of times.
Wrapping it Up
Contrary to the simplistic idea that saturated fat increases LDL and thus cardiac risk, total fat and saturated fat have a complex influence on blood lipids, the net effect of which is unclear, but is associated with a lower risk of heart attacks. These blood lipid changes persist for at least one year, so they may represent a long-term effect. It's important to remember that the primary sources of carbohydrate in the modern Western diet are wheat and sugar. Are the blood lipid patterns that associate with heart attack risk in Western countries partially acting as markers of wheat and sugar intake?
* This is why you may read that small, dense LDL is not an "independent predictor" of heart attack risk. Since it travels along with a particular pattern of HDL and triglycerides, in most studies it does not give information on cardiac risk beyond what you can get by measuring other lipoproteins.